Posted 21 Sep

Words by Sarah Keenihan.
Many of us won’t ever need her expertise. But those of us who develop diabetes may be grateful for it. If you become catastrophically burned in an accident, you could require her help too.
“I’m working on therapies to treat slow-healing skin wounds, like the ones experienced by diabetes and burns patients,” Parinaz says. “But rather than creating a treatment to apply on top of the skin, in this case the idea is to develop something that works from within.”
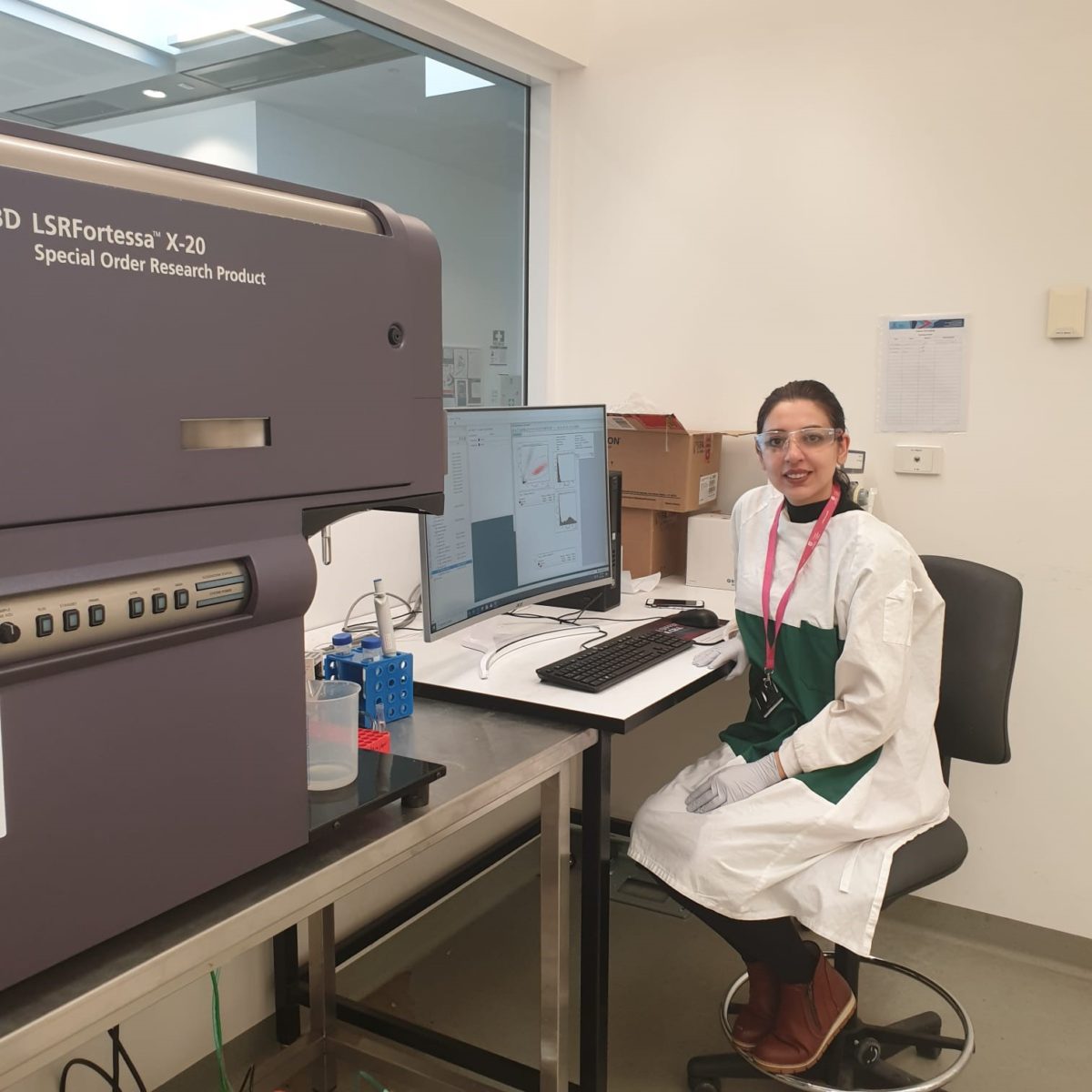
Parinaz recently completed her PhD at the Future Industries Institute at UniSA, and is now continuing her work as a postdoctoral researcher.
When healing gets stuck
In normal skin, a wound is repaired quite easily. After a cut or a scrape, the body responds with inflammation: you might see this as the affected area getting a bit red, for example. Then your body produces new skins cells, and these gradually organise themselves to cover the wound.
In diabetes, skin wounds get semi-stuck at inflammation. Even once the next steps in recovery do start to happen, they take longer too, so healing is delayed.
“A wound that would normally take around a week to heal can take up to one month or even several months to reach the same point in a person with diabetes,” says Parinaz. “The person has to manage an open wound for a long time, and infection can be a major issue.”
Slow wound healing is a serious and common problem. Around 1.9 million Australians have diabetes, and they have high risk of developing skin wounds, especially on their feet and lower limbs. Amputation is sometimes required to stop infection spreading to other parts of the body.
A new kind of therapy
You’d think the best way to improve skin healing would be to put something on it – you know, like a cream or an ointment.
“But when we talk with doctors, they say putting something on top isn’t always the best approach for managing wounds that are large and of irregular shape,” says Parinaz. “So that’s why I’m working on a different kind of therapy, something that could be injected and improve the skin wound from the inside.”
Parinaz has a specific target in mind for her new approach. It’s a molecule with an unusual name: flightless.
“flightless is a protein normally produced by our skin during inflammation and wound healing,” Parinaz explains. “But flightless levels are really high in diabetic patients with long-lasting wounds, and in other skin problems too, and we think this is part of the reason behind delayed skin healing.”
Studies show skin healing can be restored by mopping up excess flightless. This can be achieved with specific antibodies, which are molecules that stick to flightless and stop it being active.
“My current work aims to identify and test the best antibodies that block flightless,” says Parinaz. “With more experiments and eventually trials, we hope one day patients may be injected with these antibodies to treat skin wounds that don’t heal.”
In the Goldilocks zone
Skin is the largest organ in your body. Keeping the inside of your body separate from the outside might seem like a minor thing, but it’s really important. The barrier created by skin means your temperature, hydration, acidity and other key characteristics are in the “Goldilocks zone” (they’re just right) for a healthy existence.
Skin keeps germs out – most of the time – and provides you with the ability to experience touch, temperature, pressure and pain. All of these abilities help keep your body safe within your surroundings. After all, if you couldn’t feel heat you wouldn’t know when to move away from a dangerously hot fireplace, for example.
The outer layer of your skin consists mainly of dead cells, which you shed constantly.
“This is called the epidermis,” Parinaz says. “And under that is the dermis, which contains living cells plus hair follicles and glands.”
Also within the dermis are stem cells, which are immature feeder cells that can divide and mature to create new skin cells.
In her PhD work, Parinaz looked at whether focusing on stem cells could be another way to develop therapies, since low numbers of stem cells appear to be an additional problem for people with large, non-healing skin wounds.
“I found that stem cells produce different molecules which help skin recover from a wound,” Parinaz says. “My collaborators in the USA are now expanding this work to develop therapies that could be applied on or in the skin to boost repair.”
Every day, millions of people across Australia and the world are struggling to manage ongoing open wounds that compromise their health. New treatments developed by Parinaz and her colleagues may soon be able to offer new ways to mend broken skin.